Whether you’ve previously suffered cardiac arrest or have strong risk factors – our private automated implantable cardioverter defibrillator will help you carry on with life. You’ll go from anxious about your heart to carefree! Get private appointments that work around you and get the quality of your life back.
What is an automated implantable cardioverter defibrillator?
An Implantable Cardioverter Defibrillator (ICD) is a medical device that’s implanted under your skin in the chest area. The device constantly monitors the heart rhythm, and if it detects a dangerous arrhythmia, it delivers an electrical shock to the heart to restore its normal rhythm.
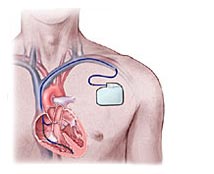
A defibrillator (ICD) is larger than a pacemaker but still goes under the skin.
Do you need an ICD?
If you’ve had a heart attack or other heart-related problems (such as an underlying heart condition), it’s strongly recommended you get an ICD implanted.
The Heart Rhythm Society has developed prevention of sudden death guidelines to help you and your physician decide whether an ICD is the best treatment for you. It’s agreed that ICD therapy is beneficial for:
- Secondary Prevention: Recommended for individuals who’ve suffered a previous cardiac arrest, or who experience spontaneous, sustained episodes of dangerous rapid heart beats that don’t self-correct.
- Primary Prevention: ICD is recommended for patients who’ve never experienced deadly heart rhythm disorders that lead to sudden cardiac death, but have significant risk factors such as poor heart pump function (ejection fraction).
What’s involved in the implantation?
The procedure is carried out in some simple steps. Please say if you are right or left-handed so the cardiologist can choose which side to place the device.
- You will be advised not to eat or drink 6 hours before your procedure.
- You’ll receive local anaesthetic and be sedated.
- Once the working area is sterile, the doctor will administer a local anaesthetic to numb the area just underneath your collarbone.
- A small cut (incision) a few inches long will be made.
- One, two or three wires called ICD leads will be advanced into your heart chambers through the veins in this area, using X-ray guidance, and stitched into position.
- The ICD generator box will be slipped under your skin or muscle and attached to these leads.
- A cardiac physiologist will test the pacing leads using a special ICD lead analyser to ensure the best lead placement.
- The ICD generator will also be tested. You will be sedated for this.
- The wound is then closed using stitches, cleaned and dressed.
- After your recovery, you will be transferred to the cardiac ward where you will stay overnight.
What happens after?
Before leaving the hospital you’ll be sent for an X-ray to confirm the position of the ICD leads. You’ll also have a pre-discharge ICD follow-up and will be prescribed a week’s course of antibiotics which you must complete.
How long does an ICD last?
The ICD now lasts at least 5-7 years. But depending on how well it’s programmed and used – often much longer. Be assured we’ll check the battery on a 6-monthly or annual basis.
Are there any risks?
ICD implantation is a routine procedure and complications are rare. However, like any surgical procedure, there’s a small degree of risk.
Possible risks include:
- Puncturing the lung or heart tissue
- Infection and bleeding around the wound site or ICD leads.
Please note: the benefits of having an ICD far outweigh the minimal risks. The primary benefit of having an ICD implant is the prevention of sudden cardiac death as a result of rhythm disturbances.
Ready to book your ICD implant?
Either give us a call, e-mail or fill out our simple contact form to arrange your consultation with London’s top cardiologist specialists.
Get seen quickly
As we’re a private clinic, your appointments work around you. You’ll soon have the answers you need so you start enjoying life again worry-free with a much better prognosis.
Pricing
Insurance
A private automated implantable cardioverter defibrillator is covered by most private medical insurance policies, but please contact your insurance company prior to your appointment to obtain your pre-authorisation code to speed things up.
Self-funding
Our price list is available on request and is on display in our waiting area. For an estimation of costs please get in touch.
Why choose London Cardiovascular Clinic?
- We offer a patient-centred approach, so you’ll feel looked after and have all your questions answered
- Choose from our flexible appointment times and get seen at your convenience
- Personalised treatment plans
- Get consultancy & treatment from London’s top cardiologists – each with their own special interests
- You’ll experience a much more welcoming and relaxing experience at our private clinic than you would elsewhere
- Video resources to help you further understand your condition and the procedures involved