Drug eluting stents (DES) have become the mainstay of treatment with coronary angioplasty, and the new generation seem safer than the previous versions, with less change of acute stent blockage with clot (stent thrombosis).
Now it seems that in acute heart attacks ( acute myocardial infarction or AMI), treated with emergency angioplasty, these DES appear to be better than older bare metal stents (BMS). The research did not look at the duration of blood thinning antiplatelet therapies, but none the less, the use of DES should be the norm, and BMS used only if there are specific risks identified that would make the DES less useful, such as high bleeding risk, or impending non-cardiac surgery.
Bmj 2014;349:g6427
Archive for 2014
what’s new with anti-platelet drugs?
Ever since since the modern era of treatment of heart attacks, we have use aspirin, blood thinning with heparins, and have hit the platelets, the cels that control clotting, with powerful drugs such as clopiodgrel, as soon as a diagnosis is suspected. That made sense when it too over a week for the cardiologist to see you and for you to get an angiogram. Now, you will be seen by cardiology within 24 hours, and will have an angiogram probably within 48 hours. So does it make sense to still give these drugs? The benefit is in reducing the chance of setting off a further heart attack. The risk is in setting of bleeding.
Recent research suggests that the pretreatment corners no benefit in terms of reducing death rate, but definately increases bleeding risk. There was a slight benefit in terms of heart attack deduction. The ACTION investigators suggest that these results will hold for those treated with stents and those with medical therapy alone. They also hold true for prasugrel or Clopiodgrel. The third big drug, Ticagrelor was not looked at.
So should we change practice? Probably not yet but we should not stress if the patient arrives without Clopiodgrel on board. We can treat once we know the anatomy on angiography. Strangely, compared to Clopiodgrel and aspirin, the combination of aspirin plus Ticagrelor has been shown to have some added benefit.
The key is to see the cardiologist! Let him/her decide.
HDL “good” Cholesterol is hard to alter
Total Cholesterol (TC), LDL-Cholesterol (Bad cholesterol), and HDL-Cholesterol (good cholesterol, are measures of lipid levesl in the blood. Which level should you focus on?
If the TC is >5 mmo/l, then think about the risk. But better is the ratio of TC :HDL. If that is >5:1 then you should worry. It should be lower, ideally <4:1.
Statins lower TC and LDL. That is good. And statins seem to do good in most people. The new NICE guidelines suggest that if your risk of heart disease over 10 years is >10%, then a statin should be considered.
Sometimes the issue is a very low HDL. Statins are not so good for that. Fibrates can do that, with some evidence that they could reduce heart attack rates, BUT NOT death rates and ONLY if not on a statin. Specific CETP inhibitors raise HDL, but appear to have NO BENEFIT at all, and one of them increased death rates.
Research by Dr Keene in my hospital suggests thatit is statins that should be considered 1st, and the others only after that- the others might affect the blood levels, but not what is important- death and heart attack rates.
BMJ 2014; 349 doi: http://dx.doi.org/10.1136/bmj.g4379 (Published 18 July 2014)
Cite this as: BMJ 2014;349:g4379
Dabigatran perhaps not as safe as expected
As with many things, something new comes along and looks great. It gets approval from the great and good, and then problems appear. It was like that for the great Thalidomide scandal more than 30 years ago. Surely it is different now?
In fact, on the back of one, large, good looking study, the RE-LY study, Dabigatran was approved as a New Oral Anticoagulant (NOAC), with the advantage of simple dosing and no blood tests needed. A recent editorial in the BMJ suggests that there remain risks, and that in fact, blood levels of the drug vary more than expected. Some have suggested that blood levels be taken.
If you are on this drug, perhaps a re-evaluation is needed? It might still be the best thing for you but…the alternatives are:
1. Warfarin
2. Rivaroxiban
3. Apixaban
4. Left Atrial appendage closure- a mini-surgical procedure to reduce stroke risk.
BMJ 2014; 349 doi: http://dx.doi.org/10.1136/bmj.g4681 (Published 23 July 2014)
Daily Express: Statins for all over-60s would slash risk of heart disease and stoke
Dr Malik comments on a recently featured study which suggests nearly everyone over the age of 60 should be given Statins to slash the risk of heart disease and stroke.
http://www.express.co.uk/life-style/health/539692/Statins-benefits-for-over-60s
Should you know your surgeons performance data?
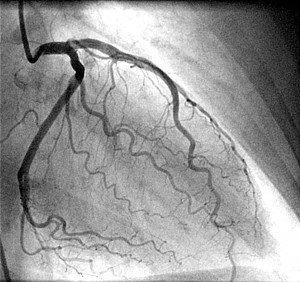
performance data for Dr Iqbal Malik 2012-2013
The medical director of the NHS, Professor Sir Bruce Keogh feels all surgeons should publish thier operative success rates. I agree, but will the general public understand that if a surgeon agrees to take on high risk cases, perhaps that others do not wish to do, then they should not be scape-goated or penalised. It is difficult to compare surgeons doing different operations on different patients.
However, you should be able to say that the surgeon does a good volume of cases. For cardiologists this sort of data has been routinely published for a few years. I attach a link to my data. I am prepared to do high risk angioplasty, including acute heart attack cases and those who have already had a cardiac arrest. Despite this my data looks good. I hope I do not become more conservative with my case selection in the future!
Dr Malik