What is a TAVi?
Transcatheter aortic valve intervention (TAVI) treats severe aortic stenosis with a minimally invasive procedure. Over the age of 75, it is not becoming the treatment of choice over conventional heart surgery.
You need careful assessment to decide
1. If you need treatment
2. How that treatment is done
Figure 1: Internal versus external dimensions
Who are Edwards Life Sciences?
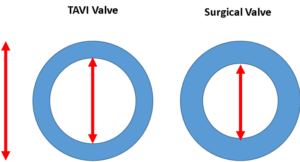
The Edwards TAVI valve is a phenomenal technology, that uses cow heart lining (Bovine pericardium) to hand make a new aortic valve, inside a metal frame.
Thus can be squashed to make it fit into a small pipe to get form the groin to the heart.
Figure 2: The Edwards S3 Ultra Resilia TAVI valve
What is a Proctor?
When other doctors are learning how to do a procedure, or have a challenging procedure where they have less experience, they can “ phone a friend”.
More formally, a Proctor can be asked to help.
By definition, a Proctor is a senior clinician, with a lot of experience in teaching and performing the procedure.
Having been a senior clinician for many years, not only have I trained doctors in my own hospital, I am a proctor for many procedures outside of my hospital, including PFO closure, ASD closure, Paravalvar leak closure, and TAVI.
Every day is a school day
I constantly learn, and this meeting was no exception.
1. Why can the Edwards valve not be squashed even smaller than the 14 French (about 5-6mm) that it is now.a. Because the collagen fibres in the cow tissue will probably be broken. And although the valve would look the same, it would not last.
2. Why cow tissue, and not horse, pig, kangaroo or some other animal?
a. Cow tissue seems to have better strength, is a bit thicker, and thus may last longer. Pig tissue is thinner, and so could be squashed more, but is more prone to tearing.
b. Edwards now have advanced tissue treatment to try to reduce calcium deposits on the valve– the main mechanism for the tissue getting stiff, and thus the TAVI valve failing. This Resilia technology is fascinating (figure 2)
3. How do we assess any residual narrowing across the new valve.
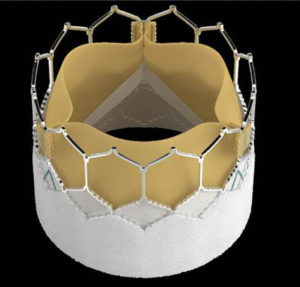
Figure 3: CT versus echo versus Invasive hemodynamics
a. It won’t be as good as the valve you are born with
b. TAVI seems to be better than a surgical valve of the same size; the external size is what is stated, and the internal size depends on the thickness of the structural material- which is thinner for TAVI than for surgical valves
c. Assessment with anatomy (really that is with CT scanning), assessment with echocardiography (using pressure gradients) and invasive pressure monitoring (at the time of TAVI) are all slightly different in the way they assess “how good” the new valve is. (Figure 3)
d. Patient –Prosthesis Mismatch (PPM) is hard to assess.
e. A residual “gradient” on echo does not necessarily mean e need top intervene- especially if there are no symptoms.
f. Flow and heart rate function are a big determinant of gradients- if the heart is weak, the gradients are low- that may not be good. If the heart is strong, the gradients may be a bit higher- more push through the same hole– that may not be bad.
4. How about if we need to do Valve in Valve TAVI?
a. Some great cases were shown, in particular on how to protect access to the coronary arteries as material is put in the way of catheters with surgical and TAVI valves
5. How about TAVI in TAVi?
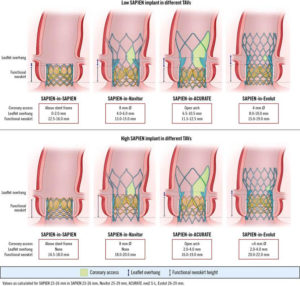
Figure 4: Putting and Edwrads TAVI inside an old TAVI
a. TAVi is so successful now, that it is likely that people who had TAVI 5-10years ago will still be alive, and the tissue in the TAVI valve will now be degenerating, and a further intervention will be needed
b. This marks a real win for TAVI, and these patients were NOT candidates for surgery back then
c. TAVI in TAVI raises its own issues, and has to be planned even more carefully than Valve in valve TAVI or TAVI in a native (your own) aortic valve. (figure 4). We need to know how to get to the coronaries, see if the old valve leaflets need to be covered or not and to see if we will block the coronary arteries completely- causing a heart attack.
Summary
It was great to share ideas with leading cardiologists and most importantly the engineers who were at the meeting.
I hope they will also take on board my use of invasive hemodymamic assessment in ALL TAVI cases, and the use of guidecatheter extensions when protecting the coronary arteries, ho hep deliver stents and imaging equipment.
Transcatheter Aortic Valve-Medtronic TAVI
Article by Dr Malik, a UK leading cardiologist. He works at One Welbeck Heart Health – London’s Largest Private Cardiology Group, and at Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, one of the largest NHS Trusts in the UK.