Air travel is generally safe for most people, but certain heart conditions may increase your risk during a flight.
At high altitudes, oxygen levels are lower, and the cabin pressure is reduced, which can place extra strain on your heart. While healthy hearts usually tolerate these changes well, some pre-existing heart issues could make flying risky. In this article, we look at what heart conditions stop you from flying, how to prepare if you’re flying with a heart condition, and when it’s best to seek medical advice before you book.
Flying with a Heart Condition
Many people with heart conditions can travel safely by plane, but some preparation is key. If you have a diagnosis or recent cardiac treatment, your first step should always be to speak with your GP or heart specialist. They’ll assess your overall stability and decide whether you’re fit to fly.
Things to consider:
- Altitude and oxygen: Aircraft cabins are pressurised, but oxygen levels remain lower than at sea level. This can affect those with reduced cardiac function or circulation issues. Some people may need in-flight oxygen, which can be arranged through the airline with prior notice.
- Destination climate: Travelling somewhere hot or cold can affect your symptoms, particularly if you take diuretics or have a fluid restriction.
- Airline policies: You may be asked to complete a fit-to-fly form or provide medical clearance if you’ve had recent treatment or require oxygen.
- Medication timing: If you’re crossing time zones, keeping to your usual medication schedule can be tricky. Bring your medicines in your hand luggage and ask your GP for guidance on adjusting timings. GTN spray (used for angina) is safe to use on board.
For peace of mind, you can arrange a private heart screening to find any potential issues in advance.
What Heart Conditions Can Stop You from Flying?
Let’s take a closer look at the main heart conditions that might restrict air travel, either temporarily or in the longer term.
Recent Heart Attack or Unstable Angina
If you’ve recently had a heart attack (myocardial infarction), your heart needs time to recover. Most people will be advised not to fly for at least 7–10 days after a mild, uncomplicated event – and longer if there were complications or if you required surgery.
Unstable angina (chest pain at rest or increasing in frequency) is another condition that makes flying unsafe. The reduced oxygen during a flight could trigger further symptoms or even a cardiac event. Until your angina is well-controlled and predictable, flying is not recommended.
Advanced Heart Failure
People with moderate to severe heart failure may struggle with reduced oxygen during a flight. If you get breathless even at rest or have had recent flare-ups or hospital admissions, you should delay travel until your condition is stable.
In-flight oxygen may be necessary even for moderate heart failure. If your symptoms only appear during exertion and are well-managed with medication, your doctor may clear you to fly, but it’s still worth planning short-haul routes and rest breaks at your destination.
Uncontrolled Arrhythmias or Serious Conduction Problems
Arrhythmias such as rapid atrial fibrillation or ventricular tachycardia can increase the risk of complications during a flight. If your heart rhythm is unstable or causing symptoms like fainting or breathlessness, you’ll likely be advised not to travel until it’s under control.
Likewise, if you’ve recently been fitted with a pacemaker or ICD, your cardiologist may recommend a short wait before flying – typically a couple of weeks, depending on your recovery. Once stable, people with these devices usually fly without issues.
Severe Valve Disease or Recent Heart Surgery
Severe valve conditions like aortic stenosis may restrict the heart’s ability to cope with stress, and the extra effort needed during flight could worsen symptoms. Travel is usually delayed until treatment is completed and the condition is stable.
If you’ve had recent heart surgery, such as valve repair or bypass surgery, you may need to wait 2–3 weeks before flying, depending on how well you’re healing. Always follow your surgeon’s advice and ensure you have any follow-up scans or checks before travelling.
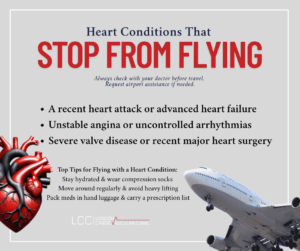
Tips for Flying with a Heart Condition
If your doctor has cleared you for air travel, the following tips can help make your journey safer and more comfortable:
- Stay hydrated: Drink plenty of water during the flight. Dehydration can increase your risk of blood clots and put extra pressure on your heart. Avoid alcohol and caffeine.
- Keep moving: Walk around the cabin when it’s safe, and do simple stretches or ankle circles in your seat. This helps circulation and reduces the risk of deep vein thrombosis (DVT).
- Wear compression socks: These can support blood flow in your legs, especially on long-haul flights.
- Bring your medicines: Keep all essential medications in your hand luggage. Carry a list of your current prescriptions, and bring extra supplies in case of delays.
- Avoid heavy lifting: Use a trolley or ask for help with your bags. Overexertion, especially in hot or stressful airport environments, can trigger symptoms.
- Plan ahead: If walking long distances is tiring, request airport assistance when booking your ticket. Let the airline know if you have a pacemaker or other medical device.
- Stick to your schedule: If travelling across time zones, ask your GP how best to manage your medication timing. Don’t skip doses.
Summary
So, what heart conditions stop you from flying? In short, any unstable, recently treated, or poorly controlled condition can make air travel risky. These include:
- A recent heart attack or advanced heart failure
- Unstable angina or uncontrolled arrhythmias
- Severe valve disease or recent major heart surgery
If you’re unsure about your condition, don’t take chances.
Book a consultation with Dr. Iqbal Malik at London Cardiovascular Clinic.
Article by Dr Malik, a leading UK cardiologist. He works at One Welbeck Heart Health – London’s Largest Private Cardiology Group, and at Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, one of the largest NHS Trusts in the UK.