On 27th September 2024, I had the privilege of attending and speaking at the TAVI Today meeting, which began with a comprehensive review of the current state of healthcare in the UK. Below are my key takeaways from the discussions:
Health and Care
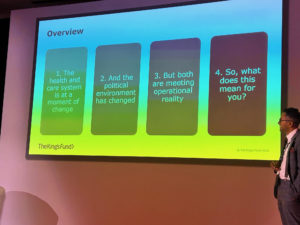
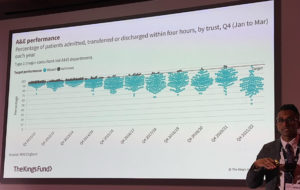
Siva Anandaciva from the King’s Fund shared how healthcare priorities have shifted. In the past, it was all about competition between institutions—financial control and meeting specific targets like four-hour A&E wait times or elective waiting lists were the focus; you could even get fired for not meeting them. These targets, however, always felt artificial.
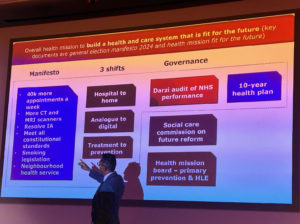
Now, the focus is on broader determinants of health, and there are three essential shifts:
- Moving care from hospitals to homes
- Transitioning from analog to digital systems
- Shifting from treatment to prevention
This is the labour manifesto—I fully agree that the three shifts are vital! However, it’s worth noting that social care still needs to be sorted out. If the door out of the hospital is blocked, with no social care, hospital beds remain full, making it impossible to admit and treat new patients.
UK TAVI Update
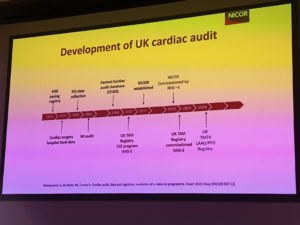
Raj Kharbanda presented an update on the UK TAVI registry, which started in 2007. It was only formally commissioned in 2023, but before that, we collected data because we, as doctors, wanted to. The registry serves two key purposes:
- Quality assurance: Are we doing a good job?
- Quality improvement: How can we do better?
Targets for TAVI procedures include:
- Performing over 200 cases annually
- Achieving more than 90% transfemoral access
- Over 90% of non-general anaesthesia cases
- Next-day discharge, with a median stay of three days
The problem, however, is that we don’t have a dedicated data entry person, and the hospital will need to fund this. The question is: How do I make it important enough for the hospital to agree?
Getting Patients to Treatment
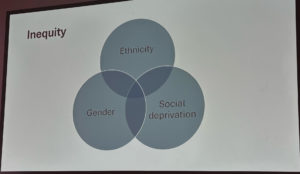
Phil MacCarthy raised an important point about inequality in access to healthcare. This inequality is based on ethnicity, gender, and social deprivation. Outreach clinics could help bridge this gap by bringing mobile valve services to the population, but we need to prove that this is both cost-effective and useful.
Day Case TAVI
At Imperial, we’ve made day-case TAVI a reality for one in five patients, which is a huge step forward. TAVI started as a major procedure, but now we’re pushing the envelope. The key is selecting patients based on social support and ECG readings, which suggests that a pacemaker is unnecessary. It’s a highly successful programme.
Long Waiting Lists: Financial Implications
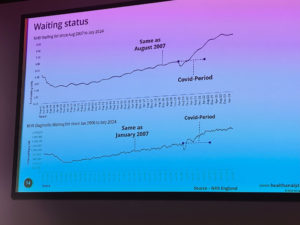
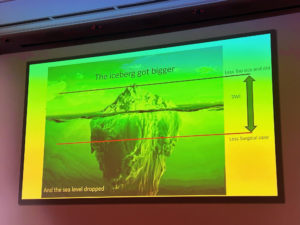
David Tuson detailed the financial side of TAVI procedures. The 18-week treatment target for cardiology is now only met in 60% of cases, and the increase in waiting times began even before TAVI became mainstream.
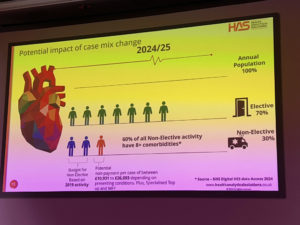
Regarding costs, the tariff pays £10,400 for an elective TAVI case and around £14,000 for a non-elective case. But here’s the catch: only contracted non-elective TAVI cases are paid. Since over 40% of the TAVI procedures we now do are non-elective, the hospital might not get paid for them. In 2018, the NHS had 20% of non-elective cases; this has now risen to 30%.
This could lead to a significant loss of income—up to £26,000 per case if we exceed the contracted volume for complex inpatient cases. It’s essential that our managers are aware of this.
The Waiting List Problem
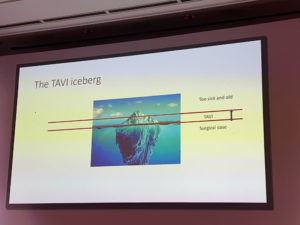
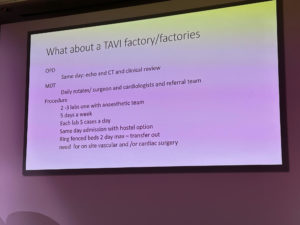
Adrian Banning discussed the ever-growing TAVI waiting list. The number of cases continues to rise, but we need to keep up. We’re very good at what we do, with only a 1% mortality rate, but we can only perform up to five TAVI procedures daily. That’s our limit.
Some have suggested expanding TAVI outside of surgical centres, but I currently disagree with that idea for a few reasons:
- We need to utilise the current resources in the bigger centres fully.
- Smaller centres need more experience.
- There is no cardiothoracic surgical cover in smaller centres.
We could consider sending other cases, like pacing and devices, to smaller centres.
There are no easy solutions here, but some of the goals we can aim for include:
- Performing a minimum of 400 TAVI procedures annually
- Allocating two TAVI days per operator
- Training an HCA to prepare the valve
- Increasing the UK TAVI volume by 100% in the next two years.
Summary
The TAVI Today meeting covered many of the key issues we know and provided some potential solutions. However, significant challenges remain, particularly around waiting lists and financial concerns, which must be addressed to ensure the system functions effectively.
You can also watch TAVI implantation by Dr Iqbal Malik- Medtronic Evolut Valve
Article by Dr Malik, a UK leading cardiologist. He works at One Welbeck Heart Health – London’s Largest Private Cardiology Group, and at Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, one of the largest NHS Trusts in the UK.