The assessment of coronary disease has changed over the years.
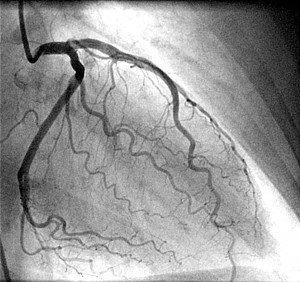
1970-1980. Angiography was the gold standard. Initially, it was done with direct aortic puncture, and generating cardiac arrest. Now it is not that risky!!! But if the cardiologist says there is a 90% stenosis, this is in fact impossible! In a 3mm vessel, a 90% stenosis would be 300micm only! This can’t be seen on the angiogram. Thus, the numbers are made up. They can help discussion with a patient, but are not accurate. Stick with mild, moderate and severe narrowings.
1980-1990. QCA- semi quantative, with a computer deciding on the angiogram how tight the narrowing is. Same issues as above, but less inter observor variability.
1990-2000. IVUS- intravasvular ultrasound has shown that the angiogram missed a lot of disease. There is no such thing as single vessel disease. The wall of all the blood vessels will be diseased.
2000-2014. Pressure and flow measurements – using wires inside the coronary arteries to look at basal readings at rest, and with drugs used to dilate the blood vessels. This was first done in animals in 1974!
What is the gold standard for detecting coronary ischaemia- muscle lacking blood in the heart?
1. Symptoms- but diabetic patients often don’t feel angina, and the history can be very variable- pain is hard to describe.
2. Exercise test- but no longer recommended in recent NICE guidelines, but may be used to give confidence to the patient and look at their exercise capacity.
3. Perfusion scanning and stress echo. These can define a lower risk group who have a negative test. But can be falsely negative and will miss smaller areas of ischaemia
4. CT scanning- this is anatomical, ie a static picture, and ischaemia at rest is rare- angina occurs on exercise usually.
5. Coronary angiography. Again anatomical.
6. Coronary invasive measurements. This is a surrogate for ischaemia as it is looking an changed blood flow, not the effect on the muscle.
-coronary flow dynamics-flow based like CFR and resistance based like HSR. It is probably coronary flow that decides how much function you have on your heart.
-coronary pressure measurements-FFR and iFR. We have been personally involved in developing the concept of iFR, which can produce a number within 3 heart beats.
7. CT FFR
– use of the techniques from invasive measurements modified to fit a non invasive technique.
Thus, there is no gold standard! So we can only look at new techniques that are proven to reduce death and heart attack rates compared to whatever the current “gold standard” is.
What is clear is that just looking at the angiogram and making a treatment decision will be flawed. We have to have other techniques available to confirm that an ugly looking narrowing is likely to cause ischaemia (the pathology), and so angina (the symptom).
What is the danger of not doing this?
-the diagnosis may be wrong. We focus on the ugly narrowing. It may have nothing to do with symptoms. It was a bystander!
-the treatment may be wrong. Especially in ostial narrowing, and branch points, the angiogram alone can overestimate the narrowing, risking inappropriate bypass surgery or stents.
Summary
This is of course where the expert opinion of the cardiologist comes in to play. Some decisions are easy, others are very tricky! We have to combine the patients risk factors, symptoms and all the test results.
Dr Iqbal Malik, Consultant Cardiologist
Dr Iqbal Malik has a CT Coronary Angiogram (CTCA) at One Welbeck Heart Health (OWHH)