I organised and moderated (chaired) the PFO session at CSI Frankfurt 2023, one of the world’s best structural heart meetings. We explored some new developments in the field and guideline updates around who will benefit from a PFO closure – with a roving microphone to stimulate discussion!
What we discussed at the PFO session
The CSI Frankfurt 2023 conference was a great opportunity to support institutions providing PFO closure by exploring the evidence base, the guidelines and any practical tips or tricks during procedures with a range of devices.
Should all PFOs be closed?
We discussed this, and no one in the room was in favour of such a strategy. The lifetime “risk” from a PFO is very low. The risk of closing it (although low risk) is NOT warranted in 25% of the population. There are many better things to spend the “healthcare dollar” on.
What do the new guidelines say about who should have a PFO procedure?
We discussed the current European/American guidelines and new guidelines that are coming soon. In short:
1. A proven stroke (with no other cause) in a younger patient.
This needs a thorough search for blood vessel hardening, blood clotting problems, and other obvious risk factors such as smoking, high blood pressure and diabetes.
2. Decompression illness (“the bends”)
It’s believed a PFO may increase the risk of decompression illness because it provides a passage for bubbles formed during a dive to bypass the lungs and directly enter the arterial circulation.
Meeting commentary
- Especially skin, neurological or vestibular
- When it is 10min to 60 min after decompression
- If you have a migraine post-dive
- Sadly, it is not covered by NHS England
Are there any alternatives?
Stopping diving or restricting your dive profile is an alternative to PFO closure (e.g. <15 m, and no heavy lifting for 3 hours after)
What does the data say?
A non-randomised study in 2011 found that:
- PFO closed: The risk is 0.5 per 10,000 dives.
- Left open: 35 per 10,000 dives
Other factors to consider
Other factors need to be considered as well, such as the size of the shunt, the diver’s profile, the nitrogen mix and your own personal risk profile. For example, if you’re overweight, there’s more space for bubbles to form in the fat.
If you do have your PFO closed, it should be retested with a bubble echo. Less than 15 bubbles shunt remaining is probably okay.
3. Orthodoxia (Platypnoea syndrome)
Orthodoxia is a rare situation when sitting up causes your O2 levels to fall. You are predisposed if you have emphysema or pulmonary hypertension. When this is the diagnosis, and due to a PFO shunt (AND NOT A SHUNT ELSEWHERE), PFO closure is curative.
4. Migraine
Migraine with aura is linked to stroke and to a PFO, but multiple trials failed to show significant benefit from PFO closure.
Meeting commentary
- I think we have not managed to pick the right patients
- NHS England does not fund it
- It might have been a stroke and not a migraine. I can close the PFO, and the migraine might get better
For information about current guidelines, please explore What is a PFO and what are the risks?
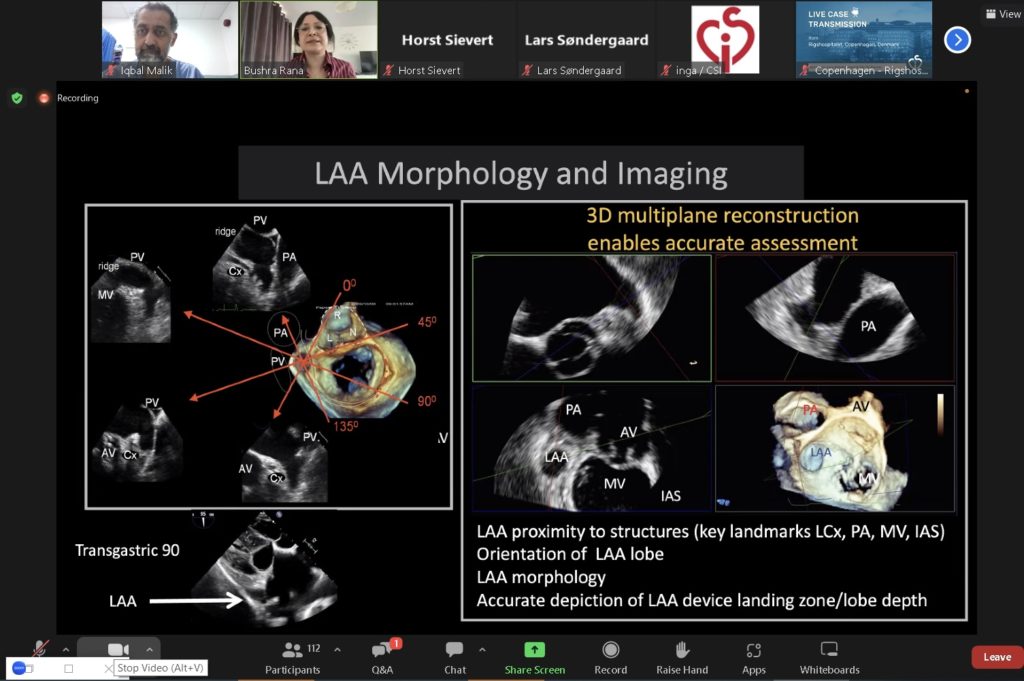
What was discussed about follow-up?
I always do a bubble echo. Given that is how we diagnose it, why would we not check with it? The majority of the CSI meeting agreed. If there is a small residual shunt it probably doesn’t matter – we agreed on that also!
What about anti-platelet medication after closure?
I continue the clopidogrel most stroke patients are on for 5 years at least and give aspirin for 1 month. There was a large variation in practice – but the majority of the meeting agreed with me, rather than those who say “the PFO was the cause” and stop the pills! I say “belt and braces “ to prevent stroke even with a successful PFO closure.
What about the over 60s?
I am waiting for a registry from Japan. They have chosen to close many older patients outside of the database of clinical trials. Given they have follow-up data on nearly 500 patients, with 30% over the age of 60, I will wait and see if they show benefit.
There is a randomised trial of older patients currently recruiting – so it may well be that it is worth it. Currently, the occasional > 60-year-old with no other risk factors, who is biologically young, can have the PFO closed if our multidisciplinary team (MDT) agrees.
What is a “high risk” PFO?
That is interesting. We discussed:
- Large shunt on valsalva – grade 3 or 4
- Hypermobile inter atrial septum – so the flap can open more
- Tunnel Length >10mm
- Eustachian Valve or Chiari network – so it directs blood to the PFO
- IVC angle low – so it points at the PFO
Final thoughts from CSI Frankfurt 2023
We think we know a lot about PFO closure, but there is always more to find out! This was one of the most impressive meetings of the year. I have been lucky enough to initially be invited as a faculty member, and now as part of the Organising Committee. It brings together some of the best of Paediatric and Adult interventional cardiology – to share learning and see new innovations.
I was very proud of my home team and enjoyed moderating the PFO session. Please see my other post about what we learnt there.
Want to book a consultation?
To ask me about PFO closure, please contact DrMalikPA@OneWelbeck.com or book your consultation.