Why Choose Dr. Iqbal Malik at London Cardiovascular Clinic?
When making a health decision, choosing the right healthcare provider is important. We offer exceptional care and expertise for PFO closure procedures at London Cardiovascular Clinic, a leading private healthcare provider in the UK.
Here’s what makes London Cardiovascular Clinic the preferred choice for a private PFO closure surgery in the UK:
- Recognised Expertise: Our team of highly skilled cardiologists, cardiac surgeons, and nurses specialises in PFO closure. Led by Dr Iqbal Malik, a leading Consultant Cardiologist, our experts bring extensive experience and a patient-centred approach to ensure the best possible outcomes. He lectures internationally on the topic and is a proctor, teaching and training cardiologists worldwide.
- Personalised Care: We understand that every patient is unique. Our dedicated team takes the time to thoroughly evaluate your condition and tailor the treatment plan to your individual needs. From the initial consultation to post-operative care, we’ll be with you every step of the way.
- Comfortable and Convenient Experience: Your well-being is our top priority. Our clinic provides a relaxed and welcoming environment, making your stay as pleasant as possible. We also offer flexible appointment scheduling to accommodate your needs, making the experience less stressful.
Is a PFO Closure Right for Me?
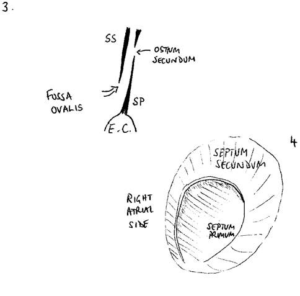
A patent foramen ovale (PFO) is a flap valve in the heart that doesn’t close properly after birth. It is needed in the womb as the baby has no use for its lungs. It closes with the 1st breath. Up to a quarter of healthy people have a PFO. While many people live with a PFO without any problems, it can increase the risk of stroke in some individuals.
Below, you can see a diagram of the PFO flap in cross-section and from the right side:
Deciding if you need a Patent Foramen Ovale closure is a personalised decision made in consultation with your doctor. They will consider several factors, including your medical history, symptoms, and individual risk factors for stroke.
According to the UK government’s NICE guidelines, a PFO closure procedure might be recommended in cases of:
- History of Stroke: If you’ve experienced a stroke, TIA or another form of ‘embolic’ event of unknown cause, especially at a young age.
- Decompression Illness: This applies to divers with recurrent paradoxical emboli, or “the bends”.
- Migraines (potentially): There’s a possible connection between PFO and migraines, but more research is needed to clarify the link. If you suffer migraines, there’s not yet a definite indication for PFO closure.
The PFO usually causes no symptoms by itself.
See how Dr. Malik performs a PFO closure on Amy Jones, a young woman who had a stroke:
How to Prepare for the PFO Closure Procedure?
Before undergoing a PFO closure procedure at the London Cardiovascular Clinic, you’ll have a comprehensive consultation with Dr. Iqbal Malik. Dr. Malik’s ability to explain complex medical problems in an easy-to-understand manner will guarantee you are well-informed throughout the process.
Before the procedure, you might undergo several tests, including:
- Electrocardiogram (ECG): This test records your heart’s electrical activity.
- Echocardiogram: This ultrasound scan creates images of your heart, allowing Dr. Malik to assess its structure and function. Injecting bubbles (agitated saline) and asking you to perform a Valsalva manoeuvre or sniff can bring out the presence of a PFO. A resting echocardiogram can easily miss a PFO. A Bubble echocardiogram is needed.
- Transoesophageal echocardiogram (TOE): This specialised echocardiogram provides detailed images of your heart, including the PFO.
- Blood tests: These tests assess your overall health and check for any underlying conditions, such as High Blood Pressure, High cholesterol, Diabetes or Anaemia.
After reviewing the results of these tests, Dr Malik will discuss with you individual instructions on how to prepare for your PFO closure. These might include dietary and/or medicinal adjustments.
What Happens During a PFO Closure?
A PFO closure procedure is minimally invasive, which means it involves a small incision rather than a large, open surgery. It is typically performed under general anaesthesia and lasts about an hour. You should be nil by mouth for 6 hours and have sips of water ONLY in that time.
Here’s a step-by-step breakdown of what you can expect:
- Preparation and Anaesthesia: You will be admitted to the ward and taken to the operating room, where a breathing tube will be placed to give the anaesthesia, and a transoesophageal echocardiogram (TOE) probe will be inserted into your stomach to guide the procedure.
- Accessing the Heart: Your cardiologist will make a small incision and insert a catheter (a thin, flexible tube) into a blood vessel in your groin, guiding it to your heart. X-rays and ultrasound images from the TOE probe will be used to navigate and position the catheter correctly.
- Measuring the PFO: A small balloon inside the catheter will measure the exact size of your foramen ovale (PFO) so Dr. Malik can choose the appropriate closure device.
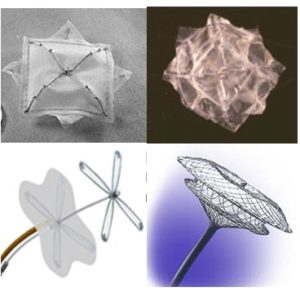
- PFO Closure Device Release: Once the catheter reaches the opening in your heart, a PFO closure device (a small, umbrella-like device made of a special nitinol mesh) is passed through the catheter. This device acts like a “cuff-link,” sealing the hole by opening an umbrella on either side.
- Completion and Recovery: The catheter and other equipment will be removed after the device is securely in place. Pressure will be applied to the puncture site in your groin to stop any bleeding.
Afterwards, you’ll be monitored for a few hours to ensure everything is alright. Patients usually go home on the same day of the procedure.
Below, you can see examples of different device options for a PFO closure procedure:
Recovery from PFO Closure
After your PFO closure procedure, you’ll receive detailed instructions on how to manage your recovery at home. This may include information about:
- Medications: You’ll likely be prescribed blood thinners to prevent blood clots from forming on the device.
- Wound Care: Instructions on how to care for the incision site to prevent infection, keeping it dry and clean.
- Physical Activity Restrictions: Guidance on when you can resume normal activities and any activities you should avoid. Typically, we advise you to take a week off work and gym workouts.
A few weeks later, you’ll attend a check-up appointment with Dr Malik. He will reassess your PFO with a bubble echocardiogram and decide if any further care is needed.
How Much Does a PFO Closure Cost?
Insurance
Most private medical insurance policies cover a private PFO closure procedure. To speed things up, please contact your insurance company before your appointment to obtain your pre-authorisation code. This will help you understand the specifics of what your policy covers and any potential out-of-pocket expenses related to the cost of PFO closure in the UK.
Self-funding
If you are self-funding your procedure, our price list is available upon request. For any estimation of costs, including the price for a private PFO closure procedure, please contact our office. We can provide detailed information and answer any questions you may have about the financial aspects of your PFO closure.
Book Your Consultation
Send us an e-mail or complete our simple contact form to arrange your consultation with London’s top cardiologist consultant, Dr Iqbal Malik.
Frequently Asked Questions
What are the risks?
This is a very safe procedure. While complications are rare, the following ones are possible:
- Bleeding: As your blood is thinned during the procedure, you could potentially suffer bleeding problems from the leg (and occasionally internally). Sometimes, blood leaks into the bag surrounding the heart, and a further procedure will be needed to help release it. Very rarely, emergency surgery is required. This is very rare.
- Heart rhythm problems: This might include palpitations (which can also just be an awareness of your heartbeat) or extra heartbeats. These usually settle with medication.
- Stroke: If a small clot forms on the device or any of the pipes and moves to the brain, you could potentially have a stroke.
- Device detachment: If the umbrella device moves, it has to be recaptured. In cases where it cannot be recaptured, you may need surgery to remove it altogether. This is again rare, as Dr Malik sizes the device carefully.
Despite the mentioned risks, the good news is that the overall complication rate is only about 1-2% after the procedure, and death is a very rare case.
To put your mind at ease, watch a video of Dr. Malik performing a PFO closure—he has been doing them for a long time!
Is PFO Closure Considered a Major Surgery?
Many patients ask if PFO closure is considered a major surgery; In fact, PFO closure is a minimally invasive procedure.
Unlike traditional open-heart surgery, PFO closure doesn’t involve large incisions. The procedure is performed using a catheter (a thin, flexible tube), which is inserted through a vein in your groin and guided to your heart. The closure device is then passed through the catheter and positioned to seal the opening.
This minimally invasive approach results in a generally quicker recovery, allowing you to resume your daily activities sooner.
What is PFO Closure Recovery Time?
A PFO closure is a minimally invasive procedure, so the recovery time is significantly shorter than open-heart surgery. Most patients can go home the same day or the day after the procedure. You can expect to feel fatigued for a few days and gradually return to your normal activities.
You’ll need to avoid strenuous activities and heavy lifting for about a week. Dr. Malik will provide you with specific instructions regarding recovery and limitations during your consultation.
It’s worth noting that complete healing takes several weeks. During this period, the device becomes fully integrated with your heart tissue. We’ll schedule follow-up appointments to monitor your progress and ensure that the closure is successful.
Is PFO Closure Cost Effective?
PFO closure, especially after a stroke, is evidence-based. Three high quality trial in 2017 all confirmed the benefit, reducing the risk of recurrent stroke by 50%, from 1% per year to 0.5% per year. When considering a medical procedure, it’s natural to weigh the cost against the potential benefits. In the case of PFO closure, research suggests that it can be a cost-effective option compared to long-term medical therapy.
A study published in the National Library of Medicine (2022) examined the cost-effectiveness of PFO closure. The results indicated that “PFO closure compared to medical therapy was estimated to have an incremental cost-effectiveness ratio (ICER) of $29,208 per quality-adjusted life year (QALY) gained, making it a cost-effective option.” This means that for every $29,208 spent, the procedure could add one year of high-quality life compared to relying solely on medication.
Further research highlighted the long-term benefits. A study published in the American College of Cardiology (2018) found that “Over a 15-year time horizon, PFO closure resulted in a gain of 0.33 QALYs at an additional cost of $7,933 compared to medical therapy, resulting in an ICER of $23,941/QALY gained.” This reinforces the idea that PFO closure is a cost-effective solution in the long run, offering patients an improvement in quality of life and a reduction in the risk of recurrent strokes.
While the initial cost of PFO closure may be higher than ongoing medical therapy, the potential for long-term benefits and improved quality of life make it a worthwhile investment. Dr. Malik at London Cardiovascular Clinic is here to help you make an informed decision based on your unique circumstances and health goals.