Dr Malik was invited to speak at the Left atrial appendage closure meeting-CSI LAA- in Frankfurt this week. He had produced a summary of the data discussed.
Who should have it?
Guidelines say that it should be for those who cannot take anti-coagulation. However, the largest Trial –PROTECT-AF- was of LAA closure with the watchman device against warfarin. And the Watchman won!
European guidelines suggest that the HASBLED (bleeding) score needs to be considered as well as the stroke risk- assessed by the CHADSVASC score.
US guidelines suggest that the Watchman could be used if the doctor thinks that LAA closure may be beneficial, if the patient is suitable for anticoagulation. The FDA has recently approved the Watchman for use in the USA. On patients suitable for warfarin.
In the UK, the funding is extremely restricted. This is limiting its use, unlike in other parts of Europe.
Cost?
In the UK, it is estimated that it costs the NHS about £7000, including the device which is about £3500.
It is cost effective, and becomes “dominant” ie cheaper and more effective, after 10 years (if comparing to Warfarin, as warfarin is cheap) or 5 years against NOAC (as these newer drugs are more expensive)
Who decides?
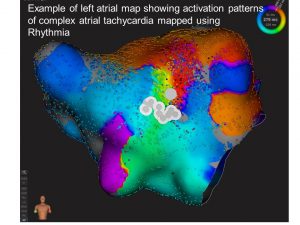
The management of AF rhythm is separate from the management of stroke risk. However, the AF does need assessment, in case it could be cured. It is worth discussing the options at a Multidisciplinary meeting to ensure that is procedure is appropriate.
What is the risk of the procedure?
• In the key trial, PROTECT-AF, the complication rate was 8%.
• In the EWOLUTION European registry of >1000 Watchman , the event rate was 1.5% only. Tamponade, bleeding around the heart was now very rare.
• In the USA registry of 3822 patients, Tamponade was in 1%, and there were 3 deaths (ie 0.1%) and thus the procedural risk is now very low. The procedure took less that 1 hour!
• In the European Amulet study of 1072 patients, there were 3 deaths (0.3%),and 0.5% pericardial effusion.
• In a study of patients who have had intracranial bleed (ICH) and so could not take anticoagulation for AF, there appeared to be a major reduction in bleed and death in a registry comparing LAA closure to medical therapy. There is now a trial staring to look at these very high risk cases.
REMEMBER: If the CHADS VASC score is 4-5, then the ANNUAL stroke risk is 5-10%! Thus doing nothing is not a safer option. If you have bypass surgery, the surgeon would rarely quote a risk of less than 1%, so the risk from LAA closure is not so extreme!.
Technical aspects:
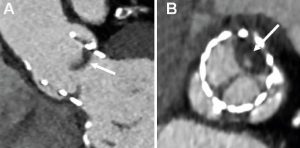
• I do it under general anaesthesia with good quality 3D transoesopgageal echo (TOE).
• Using intracardiac echo (ICE) was discussed. It avoids the general anesthetic, but the imaging is not as good as TOE. Thus I don’t use it.
• Amazing imaging such as fusing the CT image and the TOE image with the Xray was shown. Very nice, BUT not essential- I don’t use it. Having a team member doing a good quality TOE that I can see is much better than trying to to blend all the imaging on screen. I blend it in my head!
• Having the patient well hydrated was discussed. Giving fluids during the procedure might make the LAA a small difference in LAA size.
• 3D printing of the CT scan to see if you could practice the procedure is not essential. It is not going to predict what really happens!
• Types of Devices- Loads!
o Watchman
o Amplatser Cardiac Plug
o Lambre
o Occlutech LAAO
o Surgical-percutanous- Lariat
• Post procedure drugs
o No consensus on if NOAC/warfarin needed after LAA occlusion, or for how long
Overall
If you cant take anti-coagulation, you should really be considered for LAA closure. If you can, then consider NOAC like apixaban or rivaroxaban, or warfarin. A great meeting, and one that reassures me that the UK is behind the curve, and we should be offering LAA closure for more people than we are allowed to. I look forwards to doing my next live case at the next international meeting.